
Wilson’s disease is a rare genetic condition that causes the body to accumulate excessive copper due to an inability to excrete it. Copper, which is essential in trace amounts, becomes toxic when it builds up in vital organs such as the liver, brain, and eyes. Named after Dr. Samuel Wilson, who first described it in 1912, this disease is treatable if detected early, allowing patients to lead healthy lives with proper management.
Causes of Wilson’s Disease
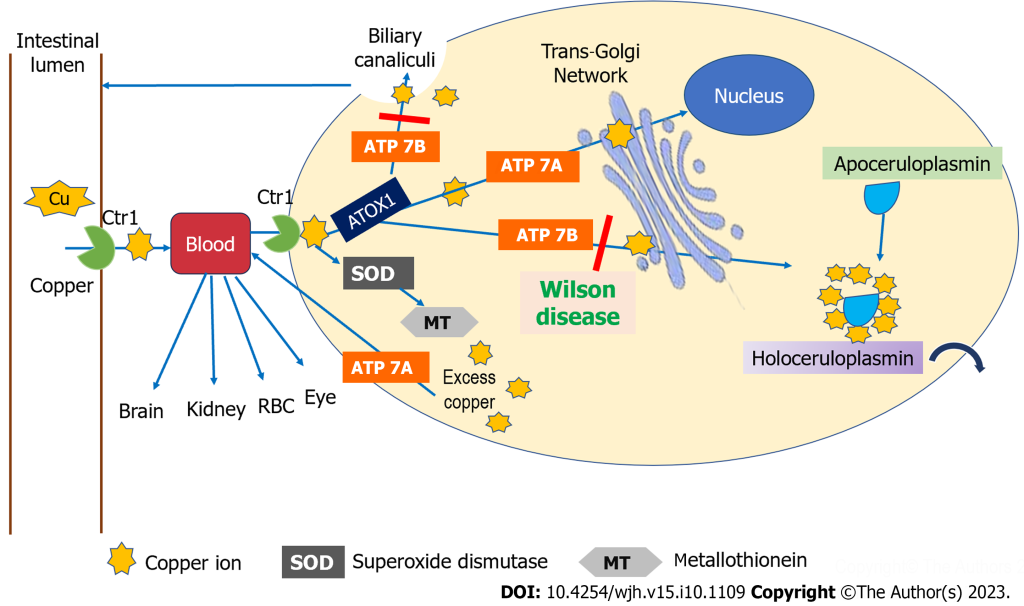
Wilson’s disease is caused by mutations in the ATP7B gene, which regulates copper transport. This defect prevents copper from being excreted into bile, leading to its buildup in the body.
Key causes include:
- Genetic Inheritance: Autosomal recessive inheritance means both parents must pass on the defective gene.
- Copper Toxicity: Excessive copper accumulates, damaging tissues in the liver, brain, and other organs.
Indications of Wilson’s Disease
Wilson’s disease can present subtly in its early stages, making diagnosis difficult. Watch for:
- Persistent fatigue and weakness.
- Jaundice or yellowing of the skin and eyes.
- Behavioral changes, including depression or irritability.
- Abdominal discomfort or swelling.
Symptoms of Wilson’s Disease
Symptoms depend on the organ affected and the stage of the disease:
- Liver Symptoms: Hepatitis, cirrhosis, and liver failure.
- Neurological Symptoms: Tremors, muscle stiffness, difficulty speaking or swallowing.
- Psychiatric Symptoms: Mood swings, anxiety, or impaired concentration.
- Eye Symptoms: Kayser-Fleischer rings, a hallmark of Wilson’s disease visible around the cornea.
Prevention Strategies of Wilson’s Disease
While Wilson’s disease cannot be prevented, early detection and proper management can reduce complications:
- Family Screening: Genetic testing for families with a history of the condition.
- Regular Monitoring: Routine tests to monitor copper levels in at-risk individuals.
- Dietary Adjustments: Avoid foods high in copper, such as shellfish, liver, and nuts.
- Timely Treatment: Adherence to prescribed therapies to prevent disease progression.
Myths and Facts About Wilson’s Disease
- Myth: Only adults are affected.
Fact: Symptoms often appear during childhood or adolescence. - Myth: Copper-rich diets cause Wilson’s disease.
Fact: It is a genetic disorder unrelated to dietary copper intake. - Myth: Treatment is only needed until symptoms improve.
Fact: Lifelong management is required to prevent relapse.
Treatments and Therapy
Medication-Based Treatments
- Chelation Therapy: Medications like penicillamine and trientine bind excess copper, helping the body excrete it.
- Zinc Therapy: Prevents copper absorption in the intestines and is often used for maintenance therapy.
Surgical Treatments
- Liver Transplantation: For patients with severe liver damage unresponsive to medical treatment.
Physical Therapy and Rehabilitation
- Improves mobility and coordination in individuals with neurological symptoms.
Lifestyle and Behavioral Interventions
- Adopting a low-copper diet and maintaining hydration are crucial for long-term management.
Alternative and Complementary Medicine
- Practices such as yoga, mindfulness, and acupuncture may provide stress relief and improve overall well-being.
Psychotherapy and Counseling
- Addresses emotional and psychological challenges associated with chronic illness.
Immunizations and Vaccines
- Prevents infections in patients with compromised liver function.
Stem Cell Therapy
- A developing area of research that may provide regenerative treatment options in the future.
Gene Therapy
- Experimental treatments aim to correct the genetic mutation, offering hope for a permanent cure.
Top 20 FAQ on Wilson’s Disease
1. What is Wilson’s disease?
A genetic disorder causing excess copper buildup in the body, primarily affecting the liver, brain, and other organs.
2. How is it diagnosed?
Wilson’s disease is diagnosed through:
- Blood tests for ceruloplasmin and copper levels.
- Liver function tests.
- Genetic screening for ATP7B mutations.
- Eye examinations for Kayser-Fleischer rings.
3. What tests confirm the disease?
Key confirmatory tests include:
- Serum ceruloplasmin levels.
- 24-hour urine copper levels.
- Liver biopsy to assess copper content.
4. Can it be cured completely?
There is no cure, but effective lifelong treatment can manage the condition and prevent complications.
5. Who is at risk?
Individuals with both parents carrying the ATP7B gene mutation have a higher risk of developing Wilson’s disease.
6. Are there lifestyle changes needed?
Yes, essential lifestyle changes include:
- Adopting a low-copper diet.
- Adhering strictly to prescribed medications.
- Regular medical follow-ups for monitoring.
7. What are Kayser-Fleischer rings?
These are copper deposits visible around the cornea, often seen during an eye exam, and are a hallmark feature of Wilson’s disease.
8. How does it affect the brain?
Wilson’s disease can cause:
- Neurological symptoms like tremors, difficulty speaking, and poor coordination.
- Psychiatric symptoms such as depression, anxiety, and personality changes.
9. Can it cause infertility?
Yes, untreated Wilson’s disease may result in hormonal imbalances and organ dysfunction, affecting fertility.
10. How is it managed during pregnancy?
Treatment is adjusted during pregnancy, with zinc therapy often emphasized to ensure safety for both the mother and baby.
11. What is the role of zinc in treatment?
Zinc therapy blocks copper absorption in the digestive system and helps maintain balanced copper levels.
12. Are there home remedies?
Home remedies like a copper-free diet and adequate hydration can support medical treatments but are not sufficient alone.
13. What foods should I avoid?
Avoid copper-rich foods, including:
- Shellfish.
- Liver.
- Nuts.
- Chocolate.
14. How long does treatment last?
Treatment is lifelong and requires regular monitoring, medications, and dietary adjustments.
15. What happens if untreated?
Untreated Wilson’s disease can lead to:
- Severe liver damage or failure.
- Neurological and psychiatric complications.
- Fatal outcomes.
16. Can children develop it?
Yes, symptoms may appear in children as young as five years old, though they are often diagnosed in adolescence.
17. Does it cause fatigue?
Yes, fatigue is a common symptom due to liver dysfunction and the toxic effects of copper buildup.
18. Is genetic testing mandatory?
Genetic testing is not mandatory but is strongly recommended for individuals with a family history of Wilson’s disease to detect carriers or affected individuals.
19. Are there new treatments available?
Ongoing research into advanced treatments, including gene therapy and stem cell therapy, offers hope for future breakthroughs.
20. Where can I get support?
Support is available through:
- Specialized clinics for Wilson’s disease.
- Patient advocacy organizations.
- Online communities and support groups for patients and families.
Conclusion
Wilson’s disease is a lifelong condition that requires awareness, early detection, and consistent management. By understanding its causes, symptoms, and treatment options, individuals and families can take control of the condition and prevent serious complications. If you or a loved one has a family history of Wilson’s disease or shows symptoms, consult a healthcare provider for early intervention.
Awareness is the key to a healthier life—act now!
Related video: